What is medical cannabis?
Medical cannabis has been a legal treatment option for patients to consider in the UK since November 2018. It must be prescribed by a specialist doctor listed on the General Medical Council’s specialist registry.
The Cannabis sativa L. genus produces active ingredients called cannabinoids, which interact with the body's endocannabinoid system (along with other receptor pathways).
This system is crucial in regulating both physiological and cognitive processes, including pain, inflammation, mood, and appetite - all of which can be issues for patients in palliative care.
What are cannabinoids?
With the global rise of medical cannabis, most people have now heard of the "big two" cannabinoids - THC and CBD.
THC is responsible for most of the psychoactive effects relating to marijuana, while CBD is non-psychoactive.
That said, both have shown enormous potential for medicinal application. Below is a brief list of just some of the potential benefits of both THC and CBD.
What are the benefits of THC and CBD in symptom management?
THC may help with:
- Pain
- Nausea
- Insomnia
- Inflammation
- Appetite stimulation
- Anxiety (at certain dosages)
- Gastrointestinal discomfort
- Muscle spasticity
CBD may help with:
- Anxiety
- Depression
- Inflammation and pain relief
- Seizures
- Nausea
- Neurodegeneration
Medical cannabis and palliative care
So, can medical cannabis play a role in palliative care?
Yes, but first, it's essential to understand that each patient's experience is different.
For some patients, traditional medications and treatments may be the best option for symptom control. For others, the addition of medical cannabis to their treatment plan is proving to be helpful.
The decision to pursue a medical cannabis prescription should be made only after consulting with a qualified specialist doctor. Here in the UK, only specialists listed on the General Medical Council's Specialist Register can legally prescribe cannabis-based medicines.
There is no one-size-fits-all approach when it comes to palliative care, and the same is true for medical cannabis treatment. Medical cannabis should never be seen as a 'magic cure'. Instead, it should be considered as part of a holistic treatment plan tailored to each patient's health needs.
With that said, despite medical cannabis currently being unlicensed in the UK due to insufficient studies and clinical trials, there is an ever-increasing body of clinical research that is slowly but surely uncovering the potential benefits that cannabis (and its many therapeutically active compounds) can offer patients suffering from a massive range of health concerns.
Can cannabis help manage pain (and inflammation) in palliative care?
Pain is, unfortunately, often at the forefront of palliative care patients' minds.
There are many different types of pain - acute, chronic, neuropathic (nerve pain), nociceptive (normal tissue injury), referred, and psychogenic. Each has its own underlying causes, and each may have a unique response to medical cannabis treatment.
As one of the most common reasons for people to reach out to their doctor, pain, and cannabis is a topic that has been studied in greater detail.
- One study evaluated chronic pain patients' views on medical cannabis. It included 984 patients with neuropathic pain, back pain, arthritis, post-surgical pain, headaches, and abdominal pain. Two-thirds of patients reported pain relief as the main benefit of cannabis.
- Another study examined the use of medical cannabis for neuropathic pain in HIV patients and found significant improvements in sleep, pain, and mood.
When it comes to inflammation specifically, CBD has shown great promise in reducing inflammatory responses by interacting with various receptors in the body responsible for immune regulation, which may lead to further pain relief.
Can cannabis help manage anxiety and depression in palliative care?
Mental health concerns often go hand-in-hand with chronic or terminal illness, and anxiety and depression are two of the most common. The burden of such a diagnosis can be overwhelming and cause immense distress, especially if the patient is facing difficult end-of-life decisions.
In terms of anxiety, the science is quite clear. Both THC and CBD have been shown to help with lowering anxiety, but in different ways and at different dosages.
This scientific review from 2017 is a good place to start. The author concluded that "Low doses of THC appear to reduce anxiety, while higher THC doses may cause increased anxiety" and that "CBD appears to decrease anxiety at all doses that have been tested".
These results are very much in line with other pieces of clinical research.
For CBD:
- This study examined anxiety related to public speaking and the impact of CBD. The results were promising, showing that a 300 mg dose could significantly reduce post-public speaking anxiety. Participants given a higher dose of 600 mg also reported much lower anxiety levels during public speaking.
- This clinical trial tested CBD's effectiveness for social anxiety disorder. Subjects received 400 mg of CBD or a placebo in a double-blind procedure. The results were promising, with CBD participants reporting significantly less anxiety compared to the control group.
There is less research to pull from regarding THC for anxiety control, but there is an abundance of anecdotal evidence. Even so, it does seem quite clear that the dosage size of THC is crucial in how it affects anxiety.
Can cannabis improve appetite and reduce nausea in palliative care patients?
Yes, medical cannabis can help with these symptoms. "The munchies" are a prominent side effect of THC, and this can be a helpful tool in stimulating the appetite of those struggling to maintain weight during palliative care.
In fact, it is a well-established treatment for nausea and appetite stimulation in cancer patients undergoing chemotherapy - one of the few 'traditional' medical applications of medical cannabis, and only one of three ways that UK patients can access cannabis-based medicines through the NHS.
- This phase II study concludes that "THC is an effective appetite stimulant in patients with advanced cancer. It is well tolerated at low doses."
- This systematic review, which looked into THC reducing vomiting and nausea in children with cancer, found "THC treatment started two hours before each antineoplastic treatment and was continued every 6 hrs for 24 hours. Vomiting was completely prevented. The side effects observed were negligible."
Can medical cannabis help palliative care patients sleep better?
Cannabis-based medications can also offer potential relief for those experiencing trouble sleeping. Life can be challenging enough as it is when dealing with a terminal illness, but add insomnia into the mix, and patients can end up feeling even more exhausted and overwhelmed.
The currently available research shows that CBD has the most potential to help with sleep issues, while THC may have mixed results depending on dosages and individual responses.
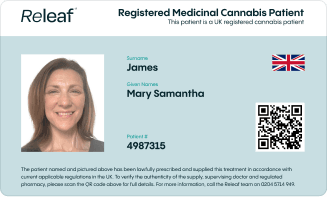
How can palliative care patients access UK medical cannabis?
In the UK, there are two routes for patients to consider regarding legal medical cannabis access.
NHS medical cannabis prescriptions
The first is through the NHS, but access to medical cannabis through this avenue is still very limited. Only patients with three specific health conditions (two rare forms of epilepsy, nausea and vomiting relating to chemotherapy treatment, or multiple sclerosis) can currently be prescribed medical cannabis by the NHS.
Even if you do have one of these health issues, the chances of receiving an NHS-funded prescription are exceedingly low.
Private medical cannabis clinics (like Releaf)
The second option, which the vast majority of UK patients currently use, is to go through a private medical cannabis clinic.
Specialist doctors working with medical cannabis clinics have more flexibility than NHS doctors when it comes to prescribing, and they can consider a far wider range of conditions on a case-by-case basis.
We offer prospective patients access to our fast and free medical cannabis eligibility checker. It takes less than one minute to complete - once done, you will have a much better idea of your likelihood of being eligible for medical cannabis treatment in the UK.
The wrap-up
To close out this write-up, we spoke to our expert palliative care specialist and Releaf medical cannabis consultant, Dr Edith Israel. Dr Israel has worked in palliative care across different settings, from the NHS and private care to hospices, for nearly 20 years.

Dr Israel said:
"The legalisation of medical cannabis and the emerging science backing up its application in clinical settings has increased the potential for cannabis-based therapy to play an important role for some patients receiving palliative care.
I have seen the impact that cannabis-based medicines can have on helping with pain, nausea, appetite, and even sleep. It is a very versatile medication that may offer relief to patients in their most difficult and vulnerable times, especially when conventional pharmaceuticals are ineffective.
While there are some concerns in terms of governance issues and policies, the changing landscape around medical cannabis means that we can work with patients to explore the potential benefits carefully and sensitively."
If you (or a loved one) would like to learn more about how medical cannabis could potentially be used during palliative care, reach out to Releaf at any time. We are passionate about advocating for the accessible and responsible application of medical cannabis to help improve the quality of life for all patients.
If you would like to learn more about cannabis-based therapy, head on over to our education hub and our blog. Both are full of valuable information and updates on the latest research and developments in this rapidly evolving field.