What is arthritis?
Rather than being a single condition or disease, arthritis refers to more than 100 conditions, including joint disease and conditions that cause joint pain. Arthritis can affect people of all ages, though some forms are more common in older individuals and among women. Some kinds of arthritis are progressive, meaning symptoms worsen over time—the two most common forms of osteoarthritis and rheumatoid arthritis.
Osteoarthritis
Osteoarthritis (OA) is the most common type of arthritis. It is estimated to affect around 10 million people in the UK alone.
OA can affect almost any joint in the body, but it most commonly affects the hands, spine, knees, and hips. This condition causes bones in the affected joints to weaken over time and the connective tissues around the joint to deteriorate, and while the exact cause of OA is unknown, factors such as injury, genetics, and other forms of arthritis may increase the risk of it developing.
Common signs and symptoms of osteoarthritis include swelling and tenderness in the joints, a grating or crackling sound when moving the joint, pain and stiffness, limited range of movement, and weakness and muscle wasting. The severity of these symptoms can vary significantly, and symptoms may come and go.
Rheumatoid arthritis
Rheumatoid arthritis is the second most common arthritic condition.
It is a type of autoimmune inflammatory arthritis in which the immune system mistakenly attacks healthy tissue in the joints. This causes the thin layer of cells covering the joints to become inflamed, releasing chemicals that damage bones, cartilage, tendons, and ligaments around the joint. It is less common than osteoarthritis, affecting an estimated 1% of the UK population.
Common symptoms of rheumatoid arthritis include pain, stiffness, and swelling around the joints. Some patients may also experience more general symptoms such as a lack of energy, high temperature, sweating, poor appetite, and weight loss. Rheumatoid arthritis can also be associated with problems in other areas of the body, including dry eyes and chest pain.
Other common types of arthritis and related conditions include:
- Cervical spondylosis - also known as degenerative osteoarthritis, affects the joints and bones in the neck.
- Ankylosing spondylitis - mainly affects the bones, muscles and ligaments of the spine.
- Psoriatic arthritis - an inflammatory joint condition that is associated with psoriasis.
- Gout - an inflammatory condition caused by excess uric acid in the body.
- Enteropathic arthritis - a type of chronic inflammatory arthritis associated with inflammatory bowel disease (IBD).
- Reactive arthritis - develops after an infection of the gut, bowel, or throat causing pain and swelling in the joints.
- Polymyalgia rheumatica - affects most people over 50 years of age. Occurs when the immune system causes muscle pain and stiffness.
What are the treatments for arthritis?
There is no cure for any kind of arthritis and treatments focus on reducing the severity and impact of symptoms. Treatments for arthritis can vary depending on the type of arthritis; however, this will usually include a combination of medications and physical therapy. In some cases, surgery may be performed to repair, strengthen, or replace the damaged joint.
Some medications for arthritis can be purchased over-the-counter, such as Acetaminophen (Tylenol), a painkiller (analgesic) often used to manage mild to moderate arthritis pain. However, stronger medications require a prescription. These include:
- Strong painkillers, including opioids
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
- Corticosteroids
- Disease-modifying antirheumatic drugs (DMARDs)
While these medications are often effective at managing pain and inflammation associated with arthritis, some may have undesirable side effects. For example, opioids have a high risk of dependence, while NSAIDs can cause headaches and dizziness, high blood pressure, and in rare cases, problems with the liver, kidneys, and heart.
Living with arthritis
Living with arthritis can present a number of challenges for patients. Decreased mobility and ability to perform everyday tasks can affect patients’ personal and professional lives, as well as relationships with friends and family. Several charities and organisations, such as Arthritis Action and Versus Arthritis, aim to provide advice and support to patients with arthritis to help them manage the physical and mental impacts of living with arthritis.
Medical cannabis and arthritis
Medical cannabis has been used for thousands of years in the treatment of a wide range of conditions. Reports from ancient Chinese, Egyptian, Indian, and Assyrian sources indicate that cannabis was used to relieve pain and inflammation, among many other ailments. However, the demonisation of the plant, beginning in the early 20th century, eventually led to the almost global prohibition of the plant.
In recent years, growing scientific and clinical evidence has added to our understanding of this complex plant and its therapeutic potential. As a result, a growing number of patients are once again looking to cannabis as a treatment option for arthritis.
How does medical cannabis help arthritis?
The cannabis plant contains hundreds of active compounds, including cannabinoids, terpenes and flavonoids. The most common cannabinoids, CBD and THC, have long been the main focus of cannabis research due to their abundance and impressive therapeutic potential.
They interact with receptors in the body’s endocannabinoid system, which are expressed throughout the central nervous system and immune system, triggering a wide range of responses. The endocannabinoid system plays a vital role in many processes, including mood and pain modulation.
The use of cannabis among patients with arthritis is thought to have been on the rise in recent years. A 2021 study of US adults with rheumatic diseases found that cannabis use among 11,006 participants increased significantly from 6.3% in 2014 to 18.4% in 2019. Of those who reported cannabis use, 74% and 62%, respectively, reported that cannabis was effective in the relief of arthritis symptoms.
While medical cannabis cannot cure arthritic conditions, a growing body of evidence indicates that it may be useful in relieving pain symptoms. Moreover, some findings indicate that cannabis-based medicines are associated with improved quality of life as well as improvements in common comorbidities of arthritis such as sleep disturbance.
Is medical cannabis safe?
Several clinical studies and systematic reviews have aimed to determine the safety and efficacy of medical cannabis in the treatment of chronic pain conditions, including arthritis. Cannabis-based medicines are consistently found to be safe and associated with few side effects, particularly when compared to conventional therapies such as opioids.
Can medical cannabis be prescribed for arthritis?
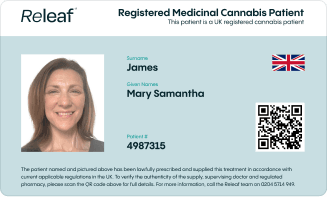
Since the UK legalised medical cannabis in 2018, specialist doctors have been able to prescribe cannabis-based medicines for a range of conditions and symptoms, including arthritis.
In fact, arthritis is the sixth-most common condition reported by Releaf patients. Under current guidelines, patients who are interested in medical cannabis for arthritis are required to have previously tried and not responded to conventional arthritis treatments.
The vast majority of patients seeking medical cannabis therapy gain a prescription through private clinics like Releaf, due to extremely low NHS medical cannabis prescription numbers. To learn more about the process of accessing medical cannabis for arthritis, find out how Releaf works.