The Home Affairs Committee Drugs report is the third Drugs report to be published during the 2022 to 2023 period, and raises two key issues when it comes to cannabis in the UK.
The first, centres around the scheduling of cannabis concerning its use as both a narcotic substance and as a medicine, whilst the second focuses on the lack of NHS prescriptions, despite their function as the nation’s health service.
Classifications, regulations, and legislations.
The legislations and regulations that dictate the scheduling of cannabis in the UK were a hot-topic during this report, with arguments ‘for’ and ‘against’ the current classification frameworks explained.
The report explains that in reality, there are no licensed cannabis based products for medicinal use in humans (CBPM) that have gained marketing authorisation from the Medicines and Healthcare Products Regulatory Agency (MHRA) or the European Medicines Agency (EMA), that satisfy the current schedule 2 definition. There are, however, unlicensed CBPMs that have not met marketing authorisation.
There are also three licensed cannabis-based medicines, named Epidyolex, Nabilone and Sativex, that do have marketing authorisation in the UK, but they are scheduled separately under the 2001 regulations, which means they are not classed as CBPMs.
This confusing classification can be incredibly difficult for patients and healthcare professionals to navigate and understand – and can instil a lot of unnecessary fear and stress for patients who are already suffering from poor health.
Professor Alex Stevens, a professor in Criminal Justice at the University of Kent and a former member of the Advisory Council on the Misuse of Drugs (ACMD), submitted his own report to be included and referenced by the Home Affairs Committee.
In his report, Professor Stevens cites that UK residents have a legal right to receive appropriate medical treatments under the Public Sector and Equality Duty, and The Humans Rights Act.
He proposed that moving medical cannabis’ classification to Schedule 4 part II of the 2001 Misuse of Drug Regulation could potentially increase access for patients in the UK that really need it.
Although still classed as controlled drugs, those on Schedule 4 part II of the 2001 legislation are legally permitted so long as they are for personal use, which is also true in the case of prescribed medical cannabis. Other substances in this category include anabolic and androgenic steroids and human growth hormones.
However, the Home Affairs Committee also explained that in November 2020 the ACMD did their own investigation and concluded that Schedule 2 remained the most appropriate classification for CBPMs.
The ACMD concluded “no further legislative amendments to the MDR regarding CBPMs are required at this point in time”, but said they would review this again in the future, should there be a marked increase in CBPMs gaining marketing authorisation.
Two years later, the government responded to this letter asking them to launch another investigation, regardless of this criteria not being met. This report was commissioned in 2022 and is expected to take approximately two years to complete.
The scarcity of NHS prescriptions
In their report, the Home Affairs Committee explained that they support CBPMs where there is an evidence base that shows its therapeutic value and efficacy in managing conditions or symptoms, and welcome the ACMD to conduct further assessments.
However, they also mention that even with the work of high profile patients like Alfie Dingley and Billy Caldwell and their families spreading awareness and influencing cannabis-based legislation in the UK, access continues to be a problem for a majority of patients.
In January 2023, Will Quince, the Minister for Health and Secondary Care, revealed that fewer than five patients have been prescribed unlicensed cannabis based products for medicinal use by NHS England since their legalisation.
Despite this taking place almost five years ago, Cannabis Health reported that a Freedom of Information Request confirmed this was still the case last month.
In comparison, over 89,000 unlicensed CBPMs were prescribed by Specialist Doctors working for private medical cannabis clinics between November 2018 and July 2022.
On this, the Committee state:
“We are concerned that there is currently a lack of access on the NHS for patient with a genuine medical need…Pending the outcome of the ACMD’s review, we recommend that the government widens the accessibility of unlicensed CBPMs on the NHS before the end of this parliament.”
With a new parliamentary session expected before January 2024, this time frame may be seen as tight to some, but to those who have been struggling to access medical cannabis since 2018, 4 months is still a long time to wait.
However, ‘before the end of this parliament’ could also refer to before the end of the next general election, with a new parliament expected to come into power in January 2025, which widens the timeframe to 16 months.
The Home Affairs Committee also stated there is evidence to suggest CBPMs can have therapeutic value when treating chronic pain, and recommends that the government invest in, or support, randomised controlled trials into their efficacy.
If these trials demonstrate CBPMs are effective, and they are deemed cost-effective, the Committee recommends the government “enables the use of CBPMs for this purpose and works with clinicians to ensure that it is a treatment option in appropriate cases”.
However, the report also highlighted that although the government has said the National Institute for Health and Care Research is open to research proposals that plan on investigating the efficacy of medical cannabis in the treatment of epilepsy, and will treat this as a priority, it ultimately should not be their responsibility.
The Committee report includes a statement from the government that reads:
“[L]ike other medicine, it is the responsibility of manufacturers to produce evidence on safety, quality and efficacy and to put forward their products for scrutiny by the Medicines and Healthcare products Regulatory Agency before a marketing authorisation (licence) is granted.
Despite calls from the [Department of Health and Social Care] Ministers, the industry has largely failed to invest in clinical trials to establish the safety, quality, and efficacy of their products.”
Reception to the Report
This report received a mixed response from those in the medical cannabis industry and advocacy spaces.
Katya Kowalski, head of operations at Volteface, was pleased to see a recognition of the real issues patients and their families in the UK face on a daily basis, but felt as though the report was lacking in recommendations.
Katya reportedly said:
“It is very positive to see the recommendations around expanding access and reducing barriers to cannabis-based medicines, as well as the recognition that the number of patients going to the illicit market to access their medicine is something that needs to be addressed.
However, they don’t provide any detail on how this should be done, so it feels like something of a throw-away comment.”
Whilst other members in the industry, such as Melissa Sturgess, Co-chair of the Cannabis Industry Council Research Working Group, felt the report made sensible suggestions.
In a Cannabis Industry Council statement released last week, Melissa said:
“Randomised control trials offer further confirmation of the known benefits of cannabis medicines. There are a number of trials already ongoing, some with financial support from the NHS. We welcome the Committee’s desire for the Government to expedite this process with additional resources and recognition.”
Her colleague, and Co-chair of the CIC Prescription Cannabis Working Group, James Smith added:
“One key way to improve accessibility is to allow GPs to prescribe cannabis medicines to their patients. The Cannabis Industry Council is running the ‘Protect our Patients’ campaign and urges politicians to support this vital change for patients.
For a wide variety of common–sense reasons, GPs must be able to initiate medical cannabis prescriptions. While we are greatly appreciative of the efforts made so far, talk is not translating into action and the lack of progress on this file is very disappointing for patients, doctors, and British industry.”
Medical Cannabis Context in the UK
The points raised by James Smith in regard to this report are thoughts shared by many members in the industry, as well as by politicians, patients, and advocates across the country.
In July, an Early Day Motion was filed by MP Crispin Blunt, asking the House of Commons to debate whether GPs should be allowed to prescribe cannabis-based treatments in appropriate circumstances.
This appeal was supported by a number of important industry organisations, such as Protect our Patients, the Cannabis Industry Council, The Medical Cannabis Clinicians Society, and has since gained 17 signatures in support from other Members of Parliament.
The Early Day Motion seeks to open up prescribing rights from the current regulatory framework that restricts the prescription of cannabis-based products to only doctors who are listed on the GMC’s specialist register.
Another topic that has recently gained political attention in the UK is an official petition that was submitted to the UK Government and Parliament, asking them to introduce ‘grow your own’ laws for medical cannabis patients.
This would entail permitting legal patients to maintain 3 to 6 flowering cannabis plants to grow their own medicine, with every patient doing so registered on a database maintained by the local council, who would inform the police of anyone legally permitted to cultivate cannabis.
At the time of writing, this petition has over 11,770 signatures – but needs 100,000 to be considered eligible for a Government response, and its closing date, the 4th of October, is fast approaching.
Closing Considerations
With medical cannabis fast approaching its five-year legalisation anniversary, it is interesting to see that these discussions are now taking place, as it is important that these issues are addressed as soon as possible.
The Home Affairs Committee report highlights significant challenges and concerns surrounding the current system, and it is evident that the scheduling and classification of cannabis creates confusion and extra hurdles for medical cannabis patients in the UK.
The lack of NHS prescriptions for medical cannabis, despite its legal status, remains a persistent issue and has left many patients unable to access the potential benefits cannabis could offer them.
The report recommendations, particularly the proposal to move medical cannabis to Schedule 4 part II, and the call for further research and investigation, holds promise for improving accessibility and improving the evidence base concerning cannabis-based treatments.
Although these are steps in the right direction, it is crucial that the government acts fast because many patients who could potentially benefit from these treatments have already waited a long time.
Politicians, policymakers, health care providers and others in the industry need to work with patients and the public to collaboratively ensure that those in need can access safe and effective medical treatments.
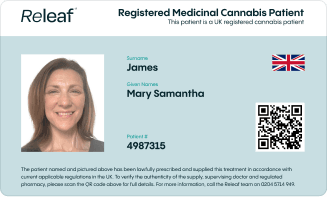
Releaf understands that embarking on your medical cannabis journey can be intimidating - that’s why we offer tailored monthly packages, specialist consultations for medical cannabis, and our unique medical cannabis card to give you the peace of mind that your treatment is protected, all based on your medical cannabis prescription.